Abstract
BACKGROUND: Pediatric-inspired regimens have been adopted by several groups as the treatment strategy for adult patients with acute lymphoblastic leukemia (ALL). Whether subsequent modifications of these protocols have led to an improvement in the outcome of patients is uncertain. This is especially relevant in T-cell ALL, where barely no new drugs have been approved in recent years. The aim of the study was to compare the outcome of patients with high risk T-cell ALL included in 2 consecutive trials of the Spanish PETHEMA Group (ALL-HR03 [NCT00853008] and the more contemporary ALL-HR11 [NCT NCT01540812]).
METHODS: Both ALL-HR03 and ALL-HR11 trials included pediatric-inspired regimens and have been published. Modifications in the ALL-HR11 protocol included a lower dose of daunorubicin in the induction phase, lower intensity of chemotherapy in the consolidation phase (except for a higher dose of MTX: 3g/m2 vs. 5g/m2) and a centralized review of minimal residual disease (MRD) by flow cytometry according to EuroFlow recommendations. In both trials, patients with poor clearance of MRD after induction or consolidation were assigned to receive allogeneic hematopoietic stem cell transplantation (allo-HSCT) in CR1 while patients with good clearance of MRD underwent subsequent delayed consolidation and maintenance with reinductions phases without allo-HSCT.
RESULTS: One-hundred and sixty-nine patients with T-cell ALL were included (104 in the HR03 and 65 in the HR11). Patient- and disease-characteristics were balanced between both groups except for a longer follow-up time in patients included in the HR03 than in the HR11 (5.2 years [range 0.1-9.1] vs. 1.8 years [0.2-4.7], p<0.001).
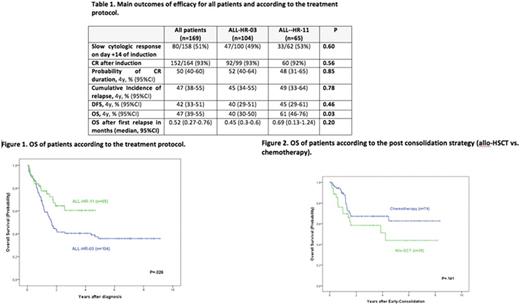
In terms of efficacy, the results are summarized in table 1. We observed a similar risk of slow cytologic response on day +14 of induction, complete remission (CR) rate and relapse in both protocols. Disease-free survival (DFS) in patients achieving CR was also similar in both groups. Patients included in the HR11 protocol had better 4-yr overall survival (OS) compared with the HR03 protocol (61% [95% CI 46%-76%] vs. 40% [95% CI 30%-50%], p = 0.026) (Figure 1).
Regarding toxicity and after censoring the follow-up at the time of transplantation, the cumulative incidence of treatment-related mortality (TRM) at 5 years for all patients was 7% (95% CI 3%-12%). More patients died of TRM during induction (7% vs. 3%) and consolidation (6% vs. 0%) in the HR03 protocol than in the HR11, respectively (p = 0.05).
Of the 152 patients achieving CR1 in both trials, 109 reached the time point for allocation to allo-HSCT in CR1 or chemotherapy (35 were assigned to allo-HSCT and 74 to chemotherapy). Patients assigned to allo-HSCT showed lower risk of relapse at 4-yrs (20% [95% CI 8%-37%] vs. 50% [95% CI 37%-62%], p = 0.005) but higher risk of TRM at 4-yrs (28% [95% CI 14%-45%] vs. 1% [95% CI 0%-7%], p < 0.001) than patients treated with chemotherapy alone. DFS at 4 years (52% [95% CI 34%-70%] vs. 49% [95% CI 36%-62%], p = 0.97) and OS at 4 years (51% [95% CI 31%-71%] vs. 67% [95% CI 55%-79%], p = 0.14) were similar in patients undergoing transplantation and chemotherapy (Figure 2).
CONCLUSIONS: Patients with T-ALL included in the HR-11 trial showed better OS than patients in the HR-03 mainly due to lower treatment-related deaths. CR rate and DFS were similar in both protocols. Promising long-term survival can be achieved in patients with T-cell ALL and good MRD clearance throughout the treatment without the need of allo-HSCT in CR1.
Montesinos: Celgene Corporation: Honoraria, Research Funding. Ribera: Celgene: Honoraria; Janssen: Honoraria; Gilead: Honoraria; Pfizer: Research Funding, Speakers Bureau; Incyte: Research Funding, Speakers Bureau; ARIAD: Research Funding, Speakers Bureau; Roche: Honoraria; Amgen Inc.: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal